Executive Summary
Before the global pandemic, there was increased conversation in the U.S. about the growth in virtual care, due in part to advances and ubiquity in technology, but also because the Centers for Medicare and Medicaid Services (CMS) reimbursement regulations were finally catching up to available technology. According to a survey conducted by HIMSS Analytics (2017), telemedicine use rose from 54% in 2014 to 71% in 2017. Now, with the COVID-19 pandemic, we are hearing even more about the explosion in telemedicine. Regulatory waivers and the potential benefits to both patients and clinicians have fostered unprecedented growth and, importantly, acceptance (and even preference) of virtual care over face-to-face office visits. According to one report, telemedicine usage increased as much as 4,330% in the few weeks after the pandemic was recognized (Mann et al., 2020).
In 2018, the Facility Guidelines Institute (FGI) Health Guidelines Revision Committee (HGRC) took a proactive approach to design for telemedicine and established requirements and recommendations for the Guidelines for Design and Construction documents for hospitals and outpatient facilities. Multiple sources were reviewed in 2014 and used as a foundation for the proposals that became the fundamental requirements and recommended appendix language for telemedicine spaces in the 2018 Guidelines. These included research studies, published industry expert opinion, and consensus documents such as association or healthcare provider standards and guidelines. This brief, originating from work developed for FGI and a 2018 article for the trade magazine Health Facilities Management (Taylor, 2018), outlines the results of that review, along with newer guidance based on the evidence that continues to emerge. While requirements for telemedicine room design are not necessarily intended to apply to virtual visits that originate from a physician’s or patient's home, some strategies can be considered in any setting, including home-based settings. To meet objectives for visual and acoustical privacy, a room is always preferred over open spaces.
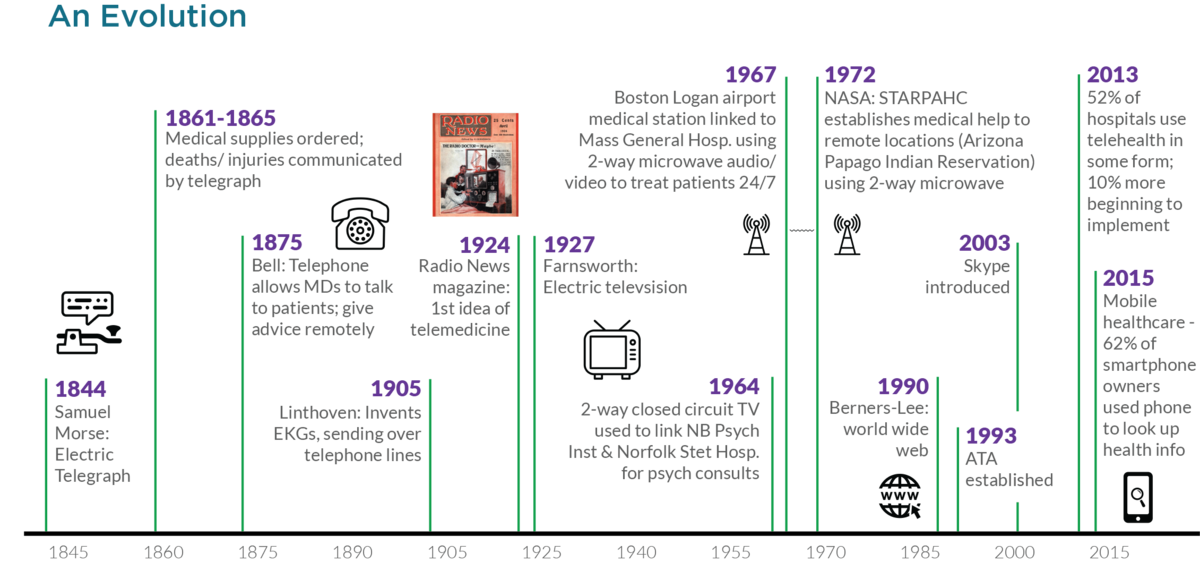
Background
By 2015, experts stated, “We are seeing telemedicine evolve from a technology‐driven novelty to an essential component of healthcare delivery in a number of specialties and fields” (Wilson & Maeder, 2015, p. 219). With stay-at-home orders in place for many U.S. locations in April 2020, the U.S. Department of Health and Human Services found that almost half (43.5%) of Medicare primary care visits were telemedicine visits compared to only a fraction of a percent (0.1%) in February 2020, prior to the declaration of a public health emergency (Bosworth et al., 2020). Now, in the midst of the global pandemic, the use of telemedicine has exploded due to waivers that have temporarily allowed physicians to employ commonly available technologies such as Zoom, Skype, and Facetime. At one Australian organization (which had seen a slow uptake in the use of telemedicine technology for the prior two years), 23 departments had at least one telehealth consultation prior to the COVID-19 pandemic, but following the declaration of the pandemic, this increased to 47 departments during April 2020 (Schulz et al., 2020). Another U.S.-based healthcare system saw non-urgent visits rise from 95 visits daily to 4,209—a 4,330% increase (Mann et al., 2020). Many of these visits are based on the patient (and even the physician) using a home-based setting to increase access to medical care, mitigate risk of disease transmission by providing for physical distancing, and conserving personal protective equipment (Hare et al., 2020).
This is dramatically different than how use was reported prior to COVID-19. According to the 2017 HIMSS Analytics survey, the largest portion of telemedicine users (30%) were one- or two-person practices. Only 24% of organizations of more than 101 physicians reported using telemedicine. The two practice types most often using telemedicine were psychiatry (21%) and pediatrics (20%). “Hub-and-spoke” platforms—those that rely on audiovisual contact within single sites (e.g., the hub hospital to the spoke hospital)—were more common for inpatient services than outpatient practices (nearly 60% compared to less than 45%). In 2019, a telemedicine survey reported that while 66% of consumers were willing to use telehealth, only 8% reported having a video visit with a doctor (Harris Poll, 2019).
Definitions
Despite an increase in the use of virtual care, many questions and inconsistencies still arise in discussions of telemedicine, including how to define the term. The origins of the term are derived from the Greek root “tele” and Latin root “medicus,” meaning “healing at a distance.” The Health Resources & Services Administration (HRSA) has defined telehealth as “the use of electronic information and telecommunication technologies to support and promote long-distance clinical health care, patient and professional health-related education, public health and health administration” (HRSA, 2017, para. 3). CMS uses the In the context of this brief, a telemedicine visit (i.e., connecting primary care or emergency department clinicians to medical specialists) differs from a more expansive use of digital telehealth (i.e., connecting clinicians to patient in their homes).
HRSA definition and the terms telehealth and telemedicine interchangeably. Recently, the ATA (American Telemedicine Association) has shifted almost exclusively to using the term telehealth compared to several years ago where they explicitly stated they used the terms interchangeably. However, in announcing their 2017 HIMSS Analytics Digital Health Pulse survey results, KPMG suggested a differentiation: “telehealth” connects clinicians directly with patients in their home or via mobile devices, while “telemedicine” connects primary care or emergency department clinicians to medical specialists via technology (KPMG, 2017). The older 2017 distinction that telemedicine is more than a home visit via mobile device is important when it comes to designing environments to support these services in the content development for the Guidelines.
While there is no shortage of technology—from two-way videos to smartphones—there is an inherent difference between connecting via FaceTime with our primary care provider when we have a cold versus coordinating patient care with specialists in another location, for patients located in underserved areas, or where it might be better to avoid unnecessary patient transfers. FGI (Facility Guidelines Institute, 2018b, p. xxxix) established a glossary definition for what the Guidelines means by telemedicine: “The use of electronic information and communications technologies to provide and support health care when distance separates the patient and medical provider.” The following note appended to the glossary definition further delineates this definition (Facility Guidelines Institute, 2018b, p. xxxix):
Clinical applications of telemedicine may encompass diagnostic, therapeutic, and forensic modalities. Common applications include pre-hospitalization assessment and post-hospital follow-up care, scheduled and urgent outpatient visits, medication management, psychotherapy, and consultation. Patient and provider consultations, medical imaging, remote monitoring, and education are all services that can be provided via telemedicine. A variety of technologies, including videoconferencing systems, internet-based websites, digital phones, and secure e-mail, can be used to deliver telemedicine services. Telemedicine facilitates the exchange of health information, services, and education between providers and providers or patients through electronic means.
In the context of this brief, a telemedicine visit differs from a more expansive use of digital telehealth with other patient-focused applications (used equally in inpatient and outpatient care), e-visit concierge services (more widely used in inpatient care), remote patient monitoring (used slightly more in outpatient care), and consumer grade off-the-shelf devices/wearables (nearly equal use in inpatient and outpatient care). In these latter platforms, the technology is more often directly connected to the patient (e.g., through a laptop) versus a fixed site (e.g., a spoke hospital)
In the context of this brief, a telemedicine visit (i.e., connecting primary care or emergency department clinicians to medical specialists) differs from a more expansive use of digital telehealth (i.e., connecting clinicians to patient in their homes).
Telemedicine services may include one-on-one interactions, consultations with a patient and family members (e.g., pediatric or elderly patients), examinations supported by a telemedicine presenter located with the patient. Specialty services (such as dermatology or orthopedics) may be provided, and each type of service may have specific needs for lighting and space to support the clinical function. Thus, it is important to know what services will be provided in the telemedicine space to achieve a functional design.
Guidelines for Designing Telemedicine Spaces
The ATA Human Factors Special Interest Group (SIG) suggests a larger context of “telepresence,” which is independent of the clinical content of the encounter. Telepresence is a synthesis of technology, environment, and human factors that encompasses the demeanor of the patient and provider along with quality of the encounter, including the ambient environment—lighting, sound/noise, and room appearance (Krupinski & Leistner, 2017).
Telemedicine requirements for the built environment were introduced in the 2018 Hospital Guidelines and Outpatient Guidelines. Requirements were included for the size of telemedicine spaces, privacy, acoustics, lighting, interior surfaces, site identification, and storage for equipment. Where low patient volume makes provision of a dedicated telemedicine room impractical, the FGI Guidelines stated a telemedicine room could also serve other functions such as a physician's office, exam room, or conference room (Facility Guidelines Institute, 2018b, 2018a).
As previously stated, it is important to note that the FGI requirements for telemedicine spaces are not intended to apply to virtual visits that do not require a physical examination of the patient or visits that originate from a physician’s or patient's home. However, with ads promoting how to “look your best” on video calls during the 2020 work-from-home lock downs, there are many strategies that are generalizable to a home setting (e.g., controlling glare, direct and indirect light).
Space Needs
Space for telemedicine should accommodate the patient, a family member and/or presenter, necessary furniture (e.g., chairs for the patient and family member, an exam table, a charting station) and equipment. According to the FGI Guidelines, where telemedicine is used for patient examination, the space must be sized so an exam table can be situated within view of the camera and the following can be accommodated: fixed or mobile telemedicine equipment, peripheral devices, an on-site caregiver or patient presenter, a hand-washing station where hands-on exams are provided, and a documentation area (Facility Guidelines Institute, 2018b).
The telemedicine room should be large enough for the patient and a patient presenter to move around comfortably for the clinical service being provided.
Additional considerations for sizing a telemedicine space in the FGI Guidelines are recommendations based on the guidance in the various reviewed sources. One of these is the proximity of the camera and microphone to the patient. The camera and exam table should be positioned so a presenter using and manipulating telemedicine peripherals can see both the patient and the monitor with images being transmitted to the remote clinician’s site (CTEConline, 2011). While some technologies (e.g. a laptop) may include embedded microphones, some organizations have opted for USB add-on omnidirectional microphones due to due to poor microphone quality on standard computers (Vilendrer et al., 2020). Space for microphones should be available in front of and close to the individuals speaking in the videoconference, ideally about 4' from the telemedicine workstation to prevent audio feedback (EMTN, 2018; PHSA, 2013). An omnidirectional microphone can be also hung from the ceiling (Krupinski et al., 2007).
The telemedicine room should be large enough for the patient and a patient presenter to move around comfortably for the clinical service being provided (CTEConline, 2011). For example, for a rheumatology examination that includes gait evaluation, the telemedicine space should be large enough for this activity to be captured by the camera (Krupinski, 2014).
Privacy
Telemedicine spaces should be designed with speech and visual privacy based on the room’s clinical function (Belz et al., 2009; Krupinski, 2014). For privacy, the space must also permit arrangement of monitors, screens, or other image or data projections so they are not visible from outside the telemedicine space. Doors can be both a distraction and a privacy concern and should be out of view of the main camera to avoid perceptions that someone might “walk in” (Major, 2005; PHSA, 2013). A separate room is preferred, and while the Guidelines only address healthcare facilities, this is also considered good practice in homes where a patient may not have not disclosed a health condition to their family and might be overheard or where family in the background become a distraction (Almathami et al., 2020).
Acoustics
Telemedicine rooms must have an acoustic environment that facilitates speech intelligibility and communication (Facility Guidelines Institute, 2018b). Hard surfaces may result in echo, reducing audio quality. As a result sound-reducing materials such as acoustical ceiling tile and carpet should be considered (CTEConline, 2011; Krupinski et al., 2007; Major, 2005). Background noise levels in telemedicine rooms must be suitable for the clinical functions performed in the space. The room should be in a quiet location that minimizes exposure to background noise that can be picked up by microphones (CTEConline, 2011). For example, locations near open office areas, busy corridors, stairwells, parking lots, waiting rooms/areas, HVAC systems, and toilet rooms are unsuitable.
Additionally, a telemedicine room also must be designed for the sound isolation rating appropriate for its clinical function. In designing to achieve the minimum Sound Transmission Coefficient (STC) rating, consideration of all portions of the room envelope is recommended, including walls, floor/ceiling assemblies, doors, and glazing as well as field conditions that may affect the performance of those elements. Specific requirements for speech intelligibility, sound isolation, and background noise are outlined in the Guidelines.
Lighting
According to the ATA, lighting is an underappreciated aspect of telemedicine encounters (Krupinski & Leistner, 2017). Given the recent focus on the importance of lighting for work-from-home video conferencing (Aten, 2020; Graham, 2020), including recommendations for “light kits” to improve appearance, awareness may have increased. However, lighting is more than “looks,” and proper lighting should ensure natural color rendition as well as even illumination levels. Lighting can contribute to clinical and social success and satisfaction in telemedicine, and should include both ambient or fill light (typically ceiling and wall-mounted) and point lighting (table lamps) to reduce shadows on participant faces (Krupinski & Leistner, 2017). Shadows (Figure 2) impact perception of skin tone, eye color, hair color, and facial expressions (Krupinski et al., 2007). While high-end cameras may have automatic gain and white point balance for correction, lower-end cameras might have limited tools to adjust image quality as lighting changes (Krupinski & Leistner, 2017) or to correct for any lighting problems (CTEConline, 2011).
(DoD photo by Fred W. Baker III [cropped])
All spaces intended for telemedicine services must allow direct frontal lighting (Major, 2005; Raymond et al., 2016). The use of both direct and indirect lighting also supports the creation of images with even lighting and accurately reproduced colors (CTEConline, 2011). If there is only one light source, the ATA Quick Guide to Telemedicine Lighting states it should be placed as close as possible and from same direction as the camera (Krupinski & Leistner, 2017). However, multiple light sources (both backlighting and fill lighting) are recommended, and the ATA Guide suggests a 60:40 ratio as the ideal balance of ceiling and wall lighting, while the California Telemedicine and eHealth Center (2011) recommends diffused light shining diagonally toward the patient to reduce shadows on the face caused by overhead lighting or a light source behind the patient or provider.
Full spectrum or warm, white light (3200–4000 K) is suggested (Krupinski & Leistner, 2017; Major, 2005; PHSA, 2013) with a minimum light level of 150 footcandles (Belz et al., 2009; Krupinski, 2014). Colored lighting (i.e., from lamp glass), as well as color inherent to the technology (e.g., narrow-spectrum blue light from an LED) should be avoided, although some specific clinical applications may call for colored room light (Krupinski & Leistner, 2017). Means for controlling glare from natural and artificial light sources is also required. For example, shades or blinds can reduce light and glare in rooms with windows (CTEConline, 2011). It should also be possible for clinicians and/or patients to avoid sitting in front of a window unless backlighting can be adequately addressed.
Gaze Angle and Camera Distance
Eye contact is an important aspect of visual communication, but when using a webcam, perceptions of eye contact are affected by the location of the camera (Chen, 2002). In videoconferencing (and telemedicine), a webcam is typically positioned on top of the monitor or laptop screen. As shown in Figure 3, the resulting angle between the eye and the camera, and the eye and the center of the display, the visual target, is the gaze angle (Grondin et al., 2019; Tam et al., 2007).
Research has established that due to our perceptions, videoconference/web cameras should be placed above the screen monitor, preferably resulting in a gaze angle less than 5º (Chen, 2002). Additional research highlights that even what might seem like insignificant changes make a difference in our perceptions. For example, when Tam and colleagues (2007) studied differences in gaze angle, they found a lower angle (7º or less) resulted in perceptions that the subject was ‘happier,’ ‘warmer,’ ‘more approachable,’ ‘more confident,’ had ‘better rapport,’ was ‘more engaged,’ and more interested in what the observer had to say. At a higher angle (15º), perceptions were more negative with perceptions that the subject was ‘reserved,’ ‘shy,’ ‘timid,’ ‘sad,’ ‘depressed,’ ‘stoned,’ ‘lost,’ ‘hiding something,’ ‘not being forthcoming,’ looking through the observer, distracted by something, not focused/engaged in the conversation, and not giving full attention.
A more recent study tested the use of a gooseneck webcam mount to lower the webcam over the edge of the monitor screen, along with a slightly raised chair height (Grondin et al., 2020). Grondin and colleagues (2020) found this allowed a decrease in the gaze angle down to 2.5°, mitigating conditions of “downward tilting” eyes that result when the webcam is mounted in a traditional location. Camera placement can also be a barrier to communication. In one study, patients felt unheard and perceived that the provider was not paying attention due to lack of eye contact when the provider looked back and forth from the computer monitors (Gordon et al., 2020).
When using a larger freestanding monitor, this may mean greater viewing distances—for example, 4'11" for a 42" monitor up to 8'2" for a 65" monitor (Ben-Arieh et al., 2016). While a “passport” picture view (head and shoulders) is suggested for introductions, the camera may subsequently be adjusted (or zoomed in/out) for a better view of the body and any non-verbal cues (Ben-Arieh et al., 2016; Grondin et al., 2019; Nguyen & Canny, 2009).
The distance between walls determines the patient to camera proximity, and this may vary by service depending on desired “framing” (how much of the head and/or body is viewed): a full view of the patient and others, a view of the upper body to recognize non-verbal cues, or just the face (Raymond et al., 2016). In some specialties, such as dermatology, there may be a need for close-up and wider views for context (ATA Teledermatology Guidelines Work Group & ATA Practice Guidelines Committee, 2016). A small room can force the camera to be located too close to the patient, limiting the clinician view (CTEConline, 2011).
are preferred
(Image courtesy Janet Major)
Framing of the view was found to be important in providing the desired “psychological” distance for both clients and therapists in telepsychotherapy (Grondin et al., 2020), as well as perceived empathy (Nguyen & Canny, 2009). The distance and range of view may influence other perceptions, as well. For example, the view of a desk in services such a telemental health is not universally accepted—some experts suggest the view of a desk can create a “buffer zone,” but others feel it may be perceived as an obstacle (Raymond et al., 2016).
Interior Surfaces
The finishes and colors selected for a telemedicine space must be able to support the natural rendition of color and pattern. All sources referenced in the development of the text were consistent in finding that light to medium blue or light gray matte finishes (Figure 4) are best for proper color rendition and facilitating picture clarity (Belz et al., 2009; CTEConline, 2011; Krupinski, 2014; Major, 2005; PHSA, 2013). These shades are preferred because they offer minimal light absorption and light reflectivity (Belz et al., 2009). If a space is used for other functions, screens or curtains may be used to provide the appropriate background color or to hide clutter (Krupinski & Leistner, 2017).
The FGI Guidelines require the backdrop wall color to have a light reflectance value of 30-40%. To avoid glare and reflections, a surface finish rating of level 1 or 2 (flat finish) is recommended rather than a gloss rating of level 5 (semi-gloss) or 6 (gloss finish). Recommendations for avoiding glare and contrast include specifying light reflectance values for surfaces: 80-90% for ceilings, 25-45% for furniture, and 20-40% for flooring (Facility Guidelines Institute, 2018b).
Site Identification
Facility identification must be provided at the telemedicine site so it appears in the transmitted image unless such identification is embedded in the electronic telemedicine platform (Figure 5). This signage is sometimes required for reimbursement but is also helpful for reminding clinicians and patients where the person they are speaking with is based when telemedicine services are offered between multiple locations (Major, 2005; PHSA, 2013).
Equipment-Associated Issues
Secure storage is required for telemedicine spaces where portable equipment and peripheral devices (e.g., digital cameras, task lighting, EKG devices, etc.) are used (Krupinski et al., 2007; PHSA, 2013). Additional guidance for equipment used for telemedicine services includes provision of temperature controls based on the heat the electronic equipment may generate (Charness et al., 2011; CTEConline, 2011); this is also a consideration for the comfort of the patient who may be unwell. Depending on the complexity of equipment used, multiple outlet types (e.g., phone, data, power) may be required (CTEConline, 2011). Locating required outlets near any equipment will mitigate the risk of hazards such as cords and cables across the floor (Charness et al., 2011). Finally, select and install telemedicine equipment to facilitate cleaning and support infection prevention practices (Krupinski et al., 2007).
the image
Conclusion
“Telehealth is not about technology, it’s about people” (Martínez-Alcalá et al., 2013). Telemedicine and telehealth have evolved quickly over the past few years, and notably, the past several months, suggesting this aspect of healthcare will now be accepted more than ever as the “new” way of doing business. As technology advances and organizations become more familiar with platforms and service options, minimum built environment standards to support these practices may need to be refined.
Language in the FGI Guidelines has been established with a small amount of verbiage as required minimum standards and more extensive recommendations in the appendix, allowing flexibility for organizations to ascertain their own level of need based on services rendered. As the industry evolves and more evidence is made available, some design requirements may also evolve with practice guidelines. However, while remote communications via electronic equipment can be a necessary supplement to in-person care, especially in a pandemic context, the design of telemedicine spaces should facilitate natural communication for the widest range of participants, including elderly patients, those unaccustomed to electronic communication, and those with vision, hearing, or cognitive impairments. Designing spaces used for telemedicine communications should always strive to maintain the level of safety, privacy, quality of care, and patient experience that would be expected for that same communication when it takes place in person.
References
Almathami, H. K. Y., Win, K. T., & Vlahu-Gjorgievska, E. (2020). Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. Journal of Medical Internet Research, 22(2), e16407. https://doi.org/10.2196/16407
ATA Teledermatology Guidelines Work Group, & ATA Practice Guidelines Committee. (2016). Practice Guidelines for TeleDermatology. https://www.americantelemed.org/resources/practice-guidelines-for-teledermatology/
Aten, J. (2020, April 13). 5 Ways to Look Your Best on Your Next Zoom Meeting. Inc.Com, online.
Belz, N., Bennett, L., Carnahan, L., Decker, V. B., Holden, D., Perry, G., Rosenthal, L., Rowe, N., Spaulding, R., Turvey, C. L., White, R., & Voyles, D. (2009). Practice Guidelines for Videoconferencing-Based Telemental Health. Telemedicine and E-Health, 17(2), 1–33. https://doi.org/10.1089/tmj.2010.0158
Ben-Arieh, D., Charness, N., Duckett, K., Krupinski, E., & Leistner, G. (2016). A Concise Guide for Telemedicine Practitioners: Human Factors Quick Guide Eye Contact (pp. 1–7) [A publication in collaboration with the Home Telehealth and Remote Monitoring SIG]. American Telemedicine Association.
Bosworth, A., Ruhter, J., Samson, L. W., Sheingold, S., Taplin, C., Tarazi, W., & Zuckerman, R. (2020). Medicare Beneficiary Use of Telehealth Visits: Early Data From The Start Of The Covid-19 Pandemic [Issue Brief]. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services.
https://aspe.hhs.gov/system/files/pdf/263866/HP_IssueBrief_MedicareTelehealth_final7.29.20.pdf
Charness, N., Demiris, G., & Krupinski, E. (2011). Designing Telehealth for an Aging Population: A Human Factors Perspective (1 edition). CRC Press.
Chen, M. (2002). Leveraging the asymmetric sensitivity of eye contact for videoconference. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, 49–56. https://doi.org/10.1145/503376.503386
CTEConline. (2011). Telemedicine Room Design (pp. 1–16). California Telemedicine and eHealth Center.
EMTN. (2018). Telemedicine Presenter Manual. Billings Clinic Eastern Montana Telemedicine Network. https://www.billingsclinic.com/app/files/public/3393/telemedicine-presenter-manual.pdf
Facility Guidelines Institute. (2018a). FGI Guidelines for Design and Construction of Hospitals. FGI.
Facility Guidelines Institute. (2018b). FGI Guidelines for Design and Construction of Outpatient Facilities. FGI.
Gordon, H. S., Solanki, P., Bokhour, B. G., & Gopal, R. K. (2020). “I’m Not Feeling Like I’m Part of the Conversation” Patients’ Perspectives on Communicating in Clinical Video Telehealth Visits. Journal of General Internal Medicine, 35(6), 1751–1758. https://doi.org/10.1007/s11606-020-05673-w
Graham, J. (2020, April 12). Six tips for looking great in a Zoom meeting. USA TODAY. https://www.usatoday.com/story/tech/2020/04/11/zoom-meetings-go-better-these-6-tips-look-your-best/5125980002/
Grondin, F., Lomanowska, A. M., Békés, V., & Jackson, P. L. (2020). A methodology to improve eye contact in telepsychotherapy via videoconferencing with considerations for psychological distance. Counselling Psychology Quarterly, 0(0), 1–14. https://doi.org/10.1080/09515070.2020.1781596
Grondin, F., Lomanowska, A. M., & Jackson, P. L. (2019). Empathy in computer-mediated interactions: A conceptual framework for research and clinical practice. Clinical Psychology: Science and Practice, 26(4), e12298. https://doi.org/10.1111/cpsp.12298
Hare, N., Bansal, P., Bajowala, S. S., Abramson, S. L., Chervinskiy, S., Corriel, R., Hauswirth, D. W., Kakumanu, S., Mehta, R., Rashid, Q., Rupp, M. R., Shih, J., & Mosnaim, G. S. (2020). COVID-19: Unmasking Telemedicine. The Journal of Allergy and Clinical Immunology: In Practice. https://doi.org/10.1016/j.jaip.2020.06.038
Harris Poll. (2019). Telehealth Index: 2019 Consumer Survey (pp. 1–13). American Well. https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf
HIMSS Analytics. (2017). HIMSS Analytics 2017 Inpatient Telemedicine Essentials: Brief Snapshot Report [Essentials Briefs]. HIMSS.
https://www.himssanalytics.org/sites/himssanalytics/files/HIMSS%20Analytics%202017%20Inpatient%20Telemedicine%20Essentials%20Brief%20Snapshot%20Report.pdf
HRSA. (2017, April 28). Telehealth Programs [Text]. Official Web Site of the U.S. Health Resources & Services Administration. https://www.hrsa.gov/rural-health/telehealth
KPMG. (2017, April). One-third of Healthcare providers use remote monitoring, “virtual care” as telemedicine evolves: KPMG Survey. https://www.prnewswire.com/news-releases/one-third-of-healthcare-providers-use-remote-monitoring-virtual-care-as-telemedicine-evolves-kpmg-survey-300441393.html
Krupinski, E. (2014). Telemedicine Workplace Environments: Designing for Success. Healthcare, 2(1), 115–122. https://doi.org/10.3390/healthcare2010115
Krupinski, E., Burdick, A., Pak, H., Bocachica, J., Edison, K., Goldyne, M., Hirota, T., Kvedar, J., McKoy, K., Oh, D., Siegel, D., Antoniotti, N., Carnahan, L., Boynton, P., Bakalar, R., Kinel, A., Kuzmak, P., Madden, B. C., Rosenthal, L., & Simmons, S. (2007). American Telemedicine Association (ATA) Teledermatology Practice Guidelines (pp. 1–25). American Telemedicine Association (ATA).
Krupinski, E., & Leistner, G. (2017). Let There Be Light: A Quick Guide to Telemedicine Lighting (pp. 1–12) [A publication in collaboration with the Home Telehealth and Remote Monitoring SIG]. American Telemedicine Association.
Major, J. (2005). Telemedicine room design. Journal of Telemedicine and Telecare, 11(1), 10–14.
Mann, D. M., Chen, J., Chunara, R., Testa, P. A., & Nov, O. (2020). COVID-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association, 27(7), 1132–1135. https://doi.org/10.1093/jamia/ocaa072
Martínez-Alcalá, C. I., Muñoz, M., & Monguet-Fierro, J. (2013). Design and Customization of Telemedicine Systems. Computational and Mathematical Methods in Medicine, 2013, 1–16. https://doi.org/10.1155/2013/618025
Nguyen, D. T., & Canny, J. (2009). More than face-to-face: Empathy effects of video framing. Proceedings of the 27th International Conference on Human Factors in Computing Systems - CHI 09, 423–432. https://doi.org/10.1145/1518701.1518770
PHSA. (2013). Telehealth Room Preparation Generic Guidelines (pp. 1–6). Provincial Health Services Authority.
Raymond, M.-C., Cornet, I., & Tanguay, L. (2016). Teleconsultation Room Design Guide. The First Nations of Quebec and Labrador Health and Social Services Commission (FNQLHSSC).
REACHhealth. (2017). 2017 U.S. Telemedicine Industry Benchmark Survey. REACH Health. https://www.healthlawinformer.com/wp-content/uploads/2017/05/2017-telemed-us-industry-survey.pdf
Schulz, T., Long, K., Kanhutu, K., Bayrak, I., Johnson, D., & Fazio, T. (2020). Telehealth during the coronavirus disease 2019 pandemic: Rapid expansion of telehealth outpatient use during a pandemic is possible if the programme is previously established. Journal of Telemedicine and Telecare, 1357633X20942045. https://doi.org/10.1177/1357633X20942045
Tam, T., Cafazzo, J. A., Seto, E., Salenieks, M. E., & Rossos, P. G. (2007). Perception of eye contact in video teleconsultation. Journal of Telemedicine and Telecare, 13(1), 35–39. https://doi.org/10.1258/135763307779701239
Taylor, E. (2018). FGI lays out telemedicine guidelines. Health Facilities Management, 31(4), 45–48.
Vilendrer, S., Patel, B., Chadwick, W., Hwa, M., Asch, S., Pageler, N., Ramdeo, R., Saliba-Gustafsson, E. A., Strong, P., & Sharp, C. (2020). Rapid deployment of inpatient telemedicine in response to COVID-19 across three health systems. Journal of the American Medical Informatics Association, 27(7), 1102–1109. https://doi.org/10.1093/jamia/ocaa077
Wilson, L. S., & Maeder, A. J. (2015). Recent Directions in Telemedicine: Review of Trends in Research and Practice. Healthcare Informatics Research, 21(4), 213–222. https://doi.org/10.4258/hir.2015.21.4.213
